Revenue Cycle Management (RCM) is the financial backbone of any healthcare provider. Poor RCM can cost a hospital up to 20% of their practical income from flaws in the billing process. From patient registration to final payment, a smooth and efficient RCM process is crucial for maintaining financial health. However, healthcare providers face numerous challenges in navigating this complex landscape. The average 250-bed hospital reports up to $11 million in lost revenue due to errors in coding and clinical documentation alone. Lumenn AI, with its “AI as your BI Team” approach, offers a powerful solution to these pain points of RCM, empowering providers to optimize their RCM and drive financial success.
Challenges Faced in Healthcare RCM
Data Silos and Inconsistent Data
Healthcare data is often fragmented across various systems (EHRs, practice management software, billing systems). This leads to data silos, preventing the exchange of fresh information across departments, and making it difficult to gain a holistic view of the revenue cycle. Healthcare organizations lose approximately 3-5% of potential revenue due to data silos and inconsistencies across systems (HFMA, 2023).
Inconsistency in data formats results in incomplete data that is unfit for analysis. Revenue cycle staff spend an estimated 30-40% of their time reconciling data discrepancies between systems rather than addressing revenue-generating activities (Healthcare Financial Management Association). Inconsistent data leads to errors and inaccurate reporting leading to rejections and delayed payment.
Denial Management and Claim Accuracy
Claim denials are a major drain on revenue. Identifying the root causes of denials and implementing corrective actions is a time-consuming and complex process. Simple mistakes—such as misspelled names, incorrect insurance IDs, or incomplete fields—can result in claim rejections. Coding errors are another significant factor contributing to claim denials. Ensuring claim accuracy and compliance with ever-changing regulations adds another layer of complexity.
Slow and Inefficient Reporting
Traditional reporting methods often rely on manual data extraction and analysis, leading to delays and inaccuracies. Organizations relying on manual data extraction across multiple systems experience an average delay of 45-60 days in identifying critical revenue cycle issues (Advisory Board Research, 2023).
Healthcare providers need timely and accurate insights into key RCM metrics, such as days in accounts receivable (A/R), denial rates, and patient payment trends.
Identifying and Addressing Revenue Leakage
Revenue leakage can occur at various stages of the RCM process, from undercoding to missed charges. Undercoding costs the average hospital $2.5-4 million annually, with evaluation and management (E&M) services being particularly vulnerable.
Detecting and preventing revenue leakage requires measures like analysis of historical coding patterns, monitoring of increased denial rates to enable targeted interventions.
Lack of Self-Service BI for No-Code Staff
RCM staff mostly lack any coding experience. They are not data analyst or BI engineers who can extract and analyze data. RCM staff already manage heavy workloads focused on claims, denials, and patient billing – they lack time to learn complex analytics systems or SQL language that most traditional BI tools depend upon. They need to be able to ask questions in natural language and receive answers quickly. Also, healthcare’s strict data governance requirements often limit what data no-code users can access and analyze.
How Lumenn AI Offers Game-Changing Solutions to RCM Challenges
Unified Data Access and Analysis
Lumenn AI allows healthcare providers to connect their data from various sources and gain a unified view of their revenue cycle. Integration of traditional BI tools to data sources of different types gets challenging as it involves migrating all data to a data lake and transforming all the data into a unique format before analysis can be done. This also poses a security and compliance issue in a highly regulated sector like healthcare.
No-code generative AI platform Lumenn AI bypasses all these steps by a technique called data federation. Your data never leaves the original storage environment and only gets connected to Lumenn. AI via universal connectors. This ensures utmost security and control over who accesses your data.
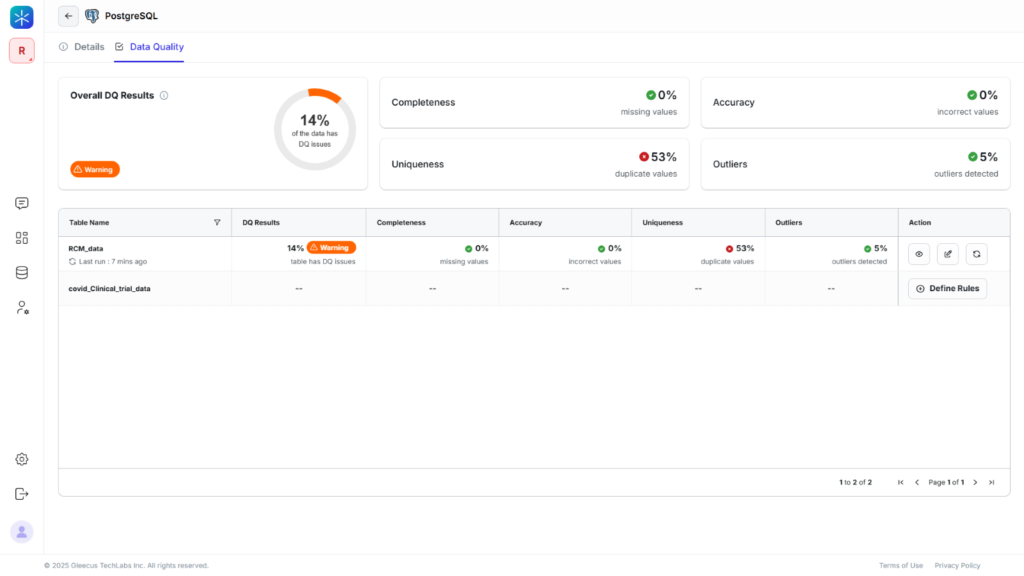
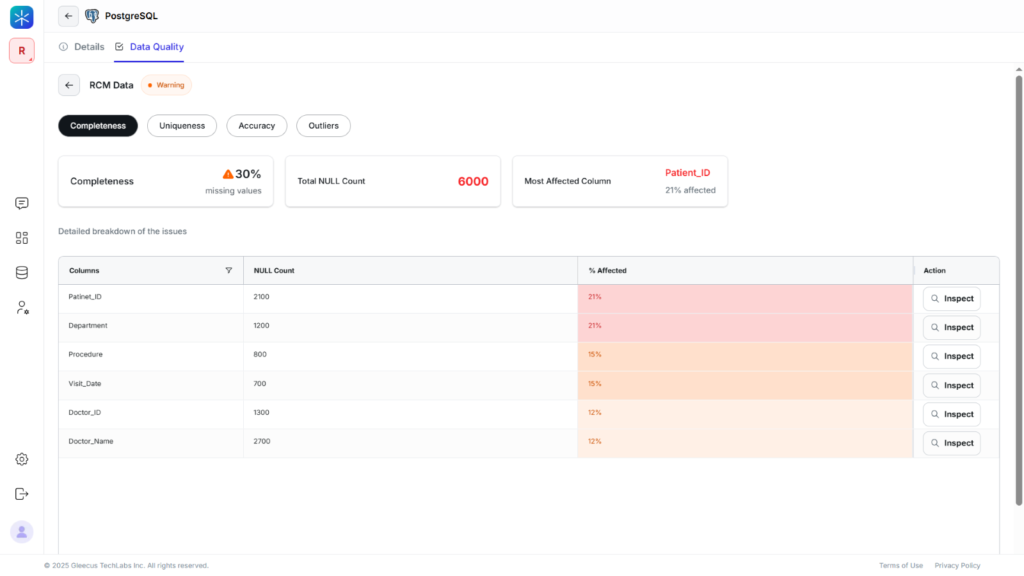
The data quality checker in Lumenn AI analyzes and rates your data for consistency, completeness and gatekeeps you run analysis on an error free data.
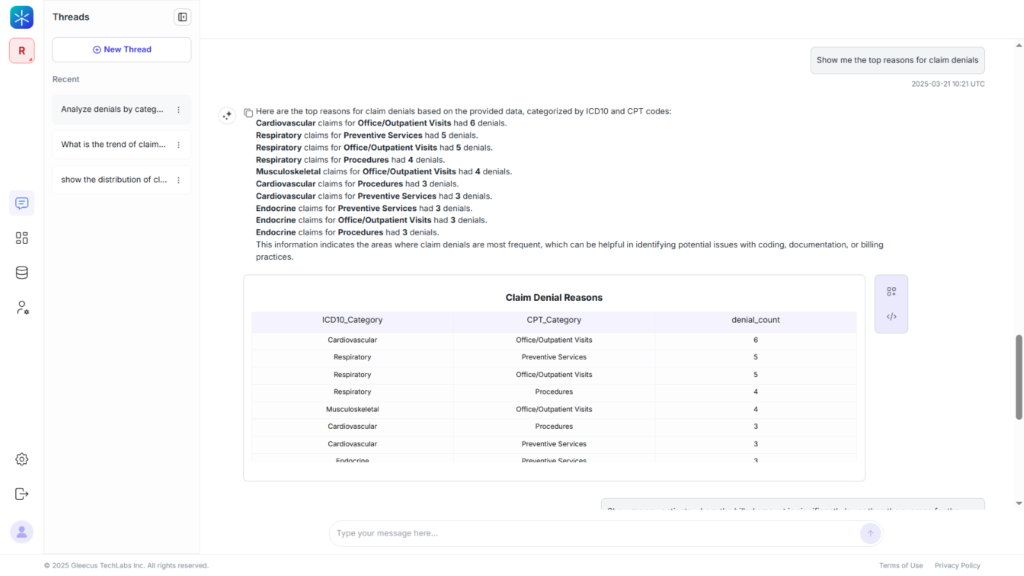
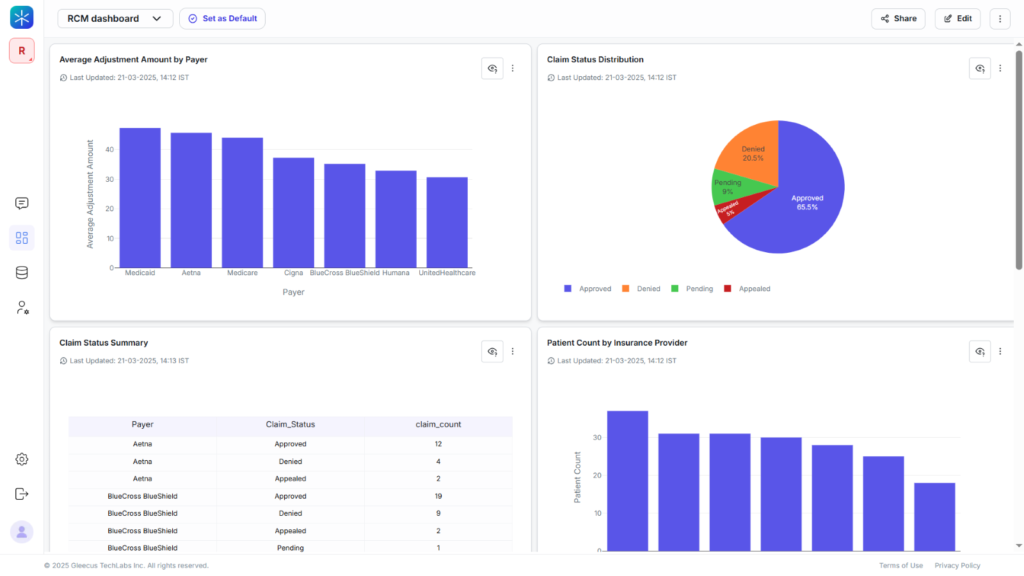
AI-Driven Denial Management
Lumenn AI leverages the power of AI algorithm to analyze patterns and anomalies that lead to claim rejection. It can generate reports and visuals to help RCM professionals and healthcare leaders get a better perception of various stages of the RCM, highlighting key denial drivers. For example, it can highlight the most common reasons for denials using pie charts or bar graphs.
AI algorithms can analyze various data points to track payer performance or categorize denials by reason (e.g., eligibility issues, coding errors). All this is done in response to Natural language queries like “Show me the top reasons for claim denials this month”. As a result, hospitals can implement targeted strategies to reduce specific types of denials.
Automated Reporting and Real-Time Insights
Lumenn AI enables healthcare providers to generate customized reports and dashboards with ease. It can easily integrate with hospital information systems (HIS), Electronic Health Records (EHR), billing systems, and other data sources to gather relevant financial and operational data. Users can ask questions like “What is our current days in A/R?” and receive instant answers. Lumenn AI dashboard maintains logs of report generation and modifications. This provides audit trails for compliance or track changes made to patient records and billing information over time.

Automating the reporting process reduces the time spent on manual data collection and report generation, allowing staff to focus on more strategic tasks. With real-time data and automated reporting, hospital administrators can make informed decisions quickly based on up-to-date financial and operational metrics.
Revenue Leakage Detection
Lumenn AI can analyze billing and coding data to identify patterns of undercoding, missed charges, and other forms of revenue leakage. It can analyze historical coding patterns, compare provider-to-provider variations, and flag encounters where documented clinical indicators suggest higher-level codes could have been used. For example, a user could ask “Show me any patients where the billed amount is significantly lower than the average for the same procedure.”
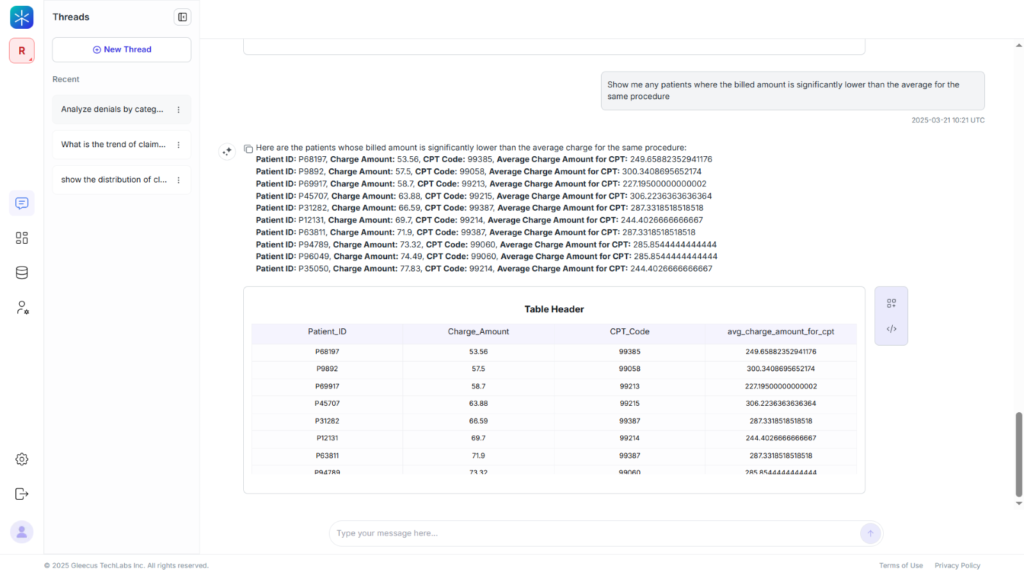
Lumenn AI excels at identifying missing charges pattern anomalies by analyzing historical service combinations and comparing provider-specific charging patterns. It shines at uncovering unidentified contractual opportunities and identifying correlations between specific coders, providers, or service types and increased denial rates, allowing targeted interventions.
Empowering No-Code Staff with Natural Language Queries
A salient feature of Lumenn AI is that it responds to natural language queries. This democratizes BI analysis and empowers the no-code staff to directly query the hospital databases and records with more trade-specific questions that an external BI or data engineer can’t guess.
Business leaders can create BI dashboards to share across teams and improve coordination. This in turn accelerates the RCM management and reduces chances of revenue leakage through undercoding or charge capture delays. Eliminating the dependency on data and BI teams frees up a good amount of opex and positively impacts the overall revenue.
Data Quality Checks for Clean Claims
Lumenn AI checks for data quality issues, such as missing patient information or incorrect coding, before claims are submitted. This helps to reduce denials and improve first-pass claim acceptance rates. The platform can provide alerts for potential data quality issues that may impact claims.
By leveraging Lumenn AI’s “AI as your BI Team” capabilities, healthcare providers can transform their RCM processes, improve financial performance, and focus on delivering quality patient care.