Hospital CEOs face the daunting task of steering their organizations toward operational excellence, financial sustainability, and superior patient outcomes. In an era where data-driven decision-making is paramount, tracking the right metrics using Business Intelligence (BI) tools is essential. This blog explores five key metrics every hospital CEO should monitor and highlights how Lumenn AI, a cutting-edge BI platform, can simplify the process.
1. Volume Metrics
Volume metrics provide insights into patient traffic and resource utilization across departments. Key indicators include:
Appointments completed per doctor
This metric measures the total number of patient appointments successfully completed by each doctor within a specified time frame, typically a month or a year.
High numbers suggest effective scheduling and patient management, while low numbers may highlight potential issues such as scheduling inefficiencies or physician availability.
Surgeries performed per surgeon
This metric tracks the total number of surgical procedures performed by each surgeon over a defined period.
A higher volume may indicate a busy practice and potentially greater expertise, while lower numbers could suggest capacity constraints or lower demand for specific surgical interventions.
Appointments scheduled per department
This metric counts the total number of appointments scheduled across different departments within the hospital.
It helps hospital leadership identify which departments are experiencing higher patient volumes and may need additional resources or staffing to meet demand effectively. Conversely, low appointment numbers in certain departments may indicate underutilization or a need for marketing efforts to attract more patients.
Why It Matters: These metrics help identify high-demand services, optimize resource allocation, and ensure that staffing levels align with patient needs.
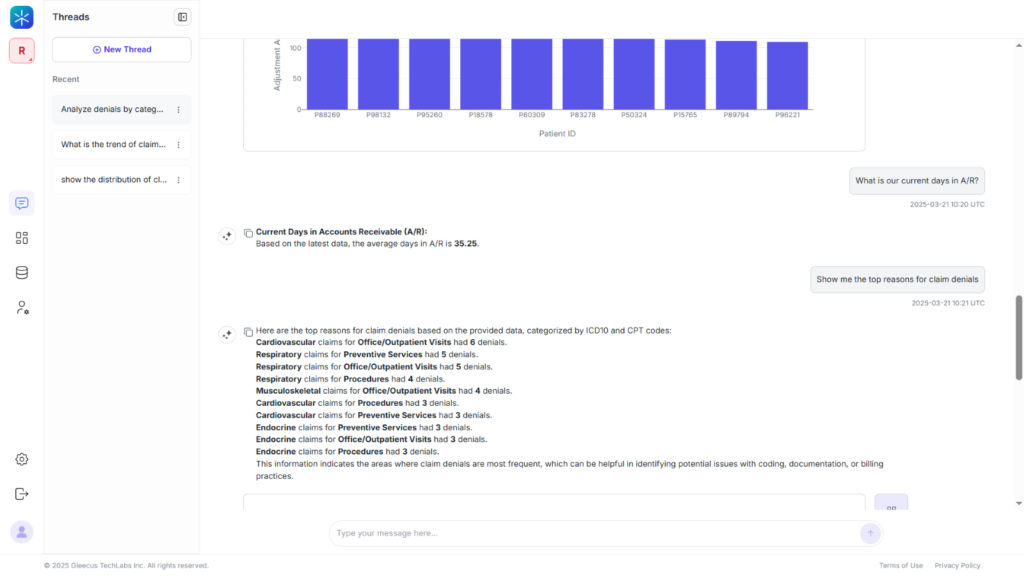
Unlocking Insights with Lumenn AI
With Lumenn AI, hospital CEOs can ask natural language queries like, “Show me the trend of surgeries performed per surgeon over the last quarter” or “Compare appointment volumes across departments.” Lumenn AI instantly generates visualizations that highlight patterns, enabling proactive adjustments to meet patient demand effectively.
2. Revenue Leakage Metrics
Revenue leakage metrics focus on identifying lost revenue opportunities within the hospital system. Examples include:
Unbilled services
Unbilled services refer to healthcare services that have been provided to patients but have not yet been billed to payers
High levels of unbilled services can negatively impact cash flow and profitability, as the hospital incurs costs for services rendered without receiving payment. Monitoring this metric helps identify areas for improvement in the revenue cycle and ensures timely billing.
Denied claims
Denied claims are requests for payment submitted to insurers that have been rejected for various reasons, such as incorrect coding, lack of prior authorization, or insufficient documentation.
Tracking denied claims is essential for identifying trends and implementing corrective actions to reduce future denials and improve overall revenue capture.
Missed charges
Missed charges refer to services or procedures that were performed but not billed due to oversight or administrative errors.
Regular monitoring of missed charges helps ensure that all services rendered are accurately captured and billed, thereby maximizing revenue.
Why It Matters: Tracking revenue leakage is crucial for maximizing financial performance and ensuring that all services rendered are appropriately billed.
Spotting Opportunities with Lumenn AI
CEOs can use Lumenn AI to query revenue data effortlessly. For instance, they could ask, “What percentage of claims were denied last month?” or “Highlight trends in missed charges over the past year.” Lumenn AI’s AI-driven insights can also flag anomalies in billing data, helping CEOs take immediate corrective actions to prevent financial losses.
3. Quality Metrics
Quality metrics evaluate care effectiveness and patient safety initiatives. Key indicators include:
Patient satisfaction scores
Patient satisfaction scores are a quantitative measure used to evaluate patients’ experiences with healthcare services.
High patient satisfaction scores often correlate with patient loyalty, better clinical outcomes, and a stronger reputation for the healthcare provider.
Readmission rates for specific conditions
Readmission rates refer to the percentage of patients who are readmitted to the hospital for the same or related condition within a specified period, typically 30 days, after their initial discharge.
Monitoring readmission rates for specific conditions helps identify opportunities to improve treatment protocols, enhance patient education, and optimize follow-up care to reduce unnecessary hospital readmissions.
Clinical outcome statistics
Clinical outcome statistics encompass a range of metrics that measure the effectiveness and impact of medical treatments and interventions on patient health. These statistics can include mortality rates, complication rates, success rates of surgical procedures, and improvements in patient health status or quality of life.
These statistics provide essential insights into the effectiveness of clinical practices, the safety of medical procedures, and the overall quality of care provided by the hospital.
Why It Matters: These metrics provide insights into care quality, helping hospitals maintain high standards and improve patient outcomes.
Enhancing Care Standards with Lumenn AI
CEOs can track quality metrics by asking questions like, “What’s the trend in patient satisfaction scores across departments?” or “Compare readmission rates for cardiac patients over the last year.” Lumenn AI’s customizable dashboards allow leaders to monitor these critical metrics in real-time and identify areas for improvement.
4. Utilization Metrics
Utilization metrics measure how effectively hospital resources are being used. Examples include:
Length of stay for patients
Length of stay (LOS) refers to the total number of days a patient spends in the hospital from admission to discharge.
LOS is a critical metric for assessing hospital efficiency and patient care quality. A shorter length of stay may indicate effective treatment and efficient discharge processes, while a longer stay could suggest complications, inefficient care pathways, or inadequate discharge planning.
Bed occupancy rates
Bed occupancy rate measures the percentage of available hospital beds that are occupied by patients at a given time.
This metric indicates how effectively a hospital is utilizing its bed capacity. High occupancy rates can reflect high demand for services but may also lead to overcrowding and strain on resources, potentially impacting patient care quality.
Resource consumption per treatment
Resource consumption per treatment measures the amount of various resources (such as staff time, medical supplies, and equipment) used to provide a specific treatment or procedure.
This metric provides insights into the efficiency and cost-effectiveness of clinical practices. High resource consumption may indicate inefficiencies or complications in treatment processes, while low consumption could suggest streamlined operations.
Why It Matters: By analyzing utilization metrics, hospitals can enhance operational efficiency, reduce costs, and maintain quality care.
Optimizing Resources with Lumenn AI
CEOs can optimize resource utilization by querying data like, “What’s our average length of stay for orthopedic patients?” or “Show me bed occupancy rates by department over the past month.” Lumenn AI’s rapid data processing enables quick identification of inefficiencies and opportunities for improvement.
5. Financial Performance Metrics
Financial performance metrics assess the hospital’s economic health. Key indicators include:
Operating margin percentage
Operating margin percentage is a financial metric that measures the proportion of revenue that remains after covering operating expenses.
This metric indicates the hospital’s operational efficiency and profitability. A higher operating margin percentage suggests that the hospital is effectively managing its costs relative to its revenue, which is crucial for financial sustainability.
Revenue growth rate
Revenue growth rate measures the percentage increase in a hospital’s revenue over a specific period.
This metric reflects the hospital’s ability to expand its services and increase its financial performance over time. A positive revenue growth rate indicates successful strategies in attracting more patients, improving service offerings, or increasing operational efficiency.
Why It Matters: Monitoring these metrics helps hospital CEOs make informed decisions about budgeting, investments, and strategic planning to ensure financial sustainability.
Gaining Financial Clarity with Lumenn AI
Financial performance can be closely monitored using queries like, “What’s our current operating margin compared to last quarter?” or “Show me revenue growth trends over the past year.” Lumenn AI integrates multiple data sources seamlessly to provide a comprehensive analysis without requiring complex data manipulation.
Why Lumenn AI Is the Ideal BI Tool for Hospital CEOs
Lumenn AI empowers hospital CEOs by addressing common challenges in tracking these metrics:
- Unified Data Integration: Connects seamlessly with multiple data sources like EMRs and billing systems.
- Real-Time Insights: Analyzes real-time data and delivers reports and visualization instantly responding to natural language prompts.
- AI as BI Team: Identifies trends and anomalies automatically, ensuring proactive decision-making.
- Customizable Dashboards: Allows CEOs to track both quality and financial metrics side-by-side.
- No-Code Interface: Eliminates reliance on technical teams by enabling users to ask questions in plain language.
- Secured Data: Just connects to the data sources using universal connectors without copying or migrating data.
Conclusion: Drive Success with Data-Driven Decisions
Tracking these five key metrics is vital for hospital CEOs to optimize operations, improve patient outcomes, and ensure financial sustainability. With Lumenn AI’s intuitive interface and powerful analytics capabilities, hospital leaders can unlock actionable insights effortlessly—empowering them to make informed decisions that drive success.